Aloe vera (Aloe barbadensis) has been proven by research to inhibit (stop the growth of) many types of fungus. Fungi causing ringworm (tinea), yeast infections, and nail infections are inhibited by Aloe vera. So if one of these common superficial fungal infections is what you want to treat; then, Aloe vera should help to some degree.
It is important to understand, in the research we will cover in this article and in real life applications, the preparation of Aloe vera you use is important. Research seems to indicate that ethanol (drinking alcohol) extracts of this herb are more potent antifungals than their water-based counterparts.
Extracts also in general may be more effective than the gel or juice of the Aloe vera leaves. Extracts contain concentrated levels of phytochemicals (plant chemicals) present in this herb. And, you may not see positive effects with just Aloe vera gel.
Instead, for the most effective Aloe vera treatment, consider buying or making an extract of Aloe vera—preferably ethanolic. And, if you do make an extract, remember not to use it internally without consulting a medical professional. Extracts are often much more potent, and dangerous, than the unprocessed herb.
But, in general, Aloe vera in all preparations probably imparts some degree of antifungal ability against many common fungi causing yeast infections, ringworm, and nail infections. Yet, to get the most benefit, consider mixing in other antifungal herbs. For topical preparations, you can also add some antifungal essential oils.
By expanding your remedy to be more than just Aloe vera gel or extract, you should see superior results.
Dr. John Herzog (MD)
Dr. John Herzog, a "survival surgeon" from Maine explains what home remedies work best in a crisis situation.
This may be important in the event you require first-aid or are in an emergency situation without easy access to a hospital. Dr. John Herzog has assembled a large collection of home remedies for such scenarios.

Aloe vera’s Effects on Ringworm (Tinea)
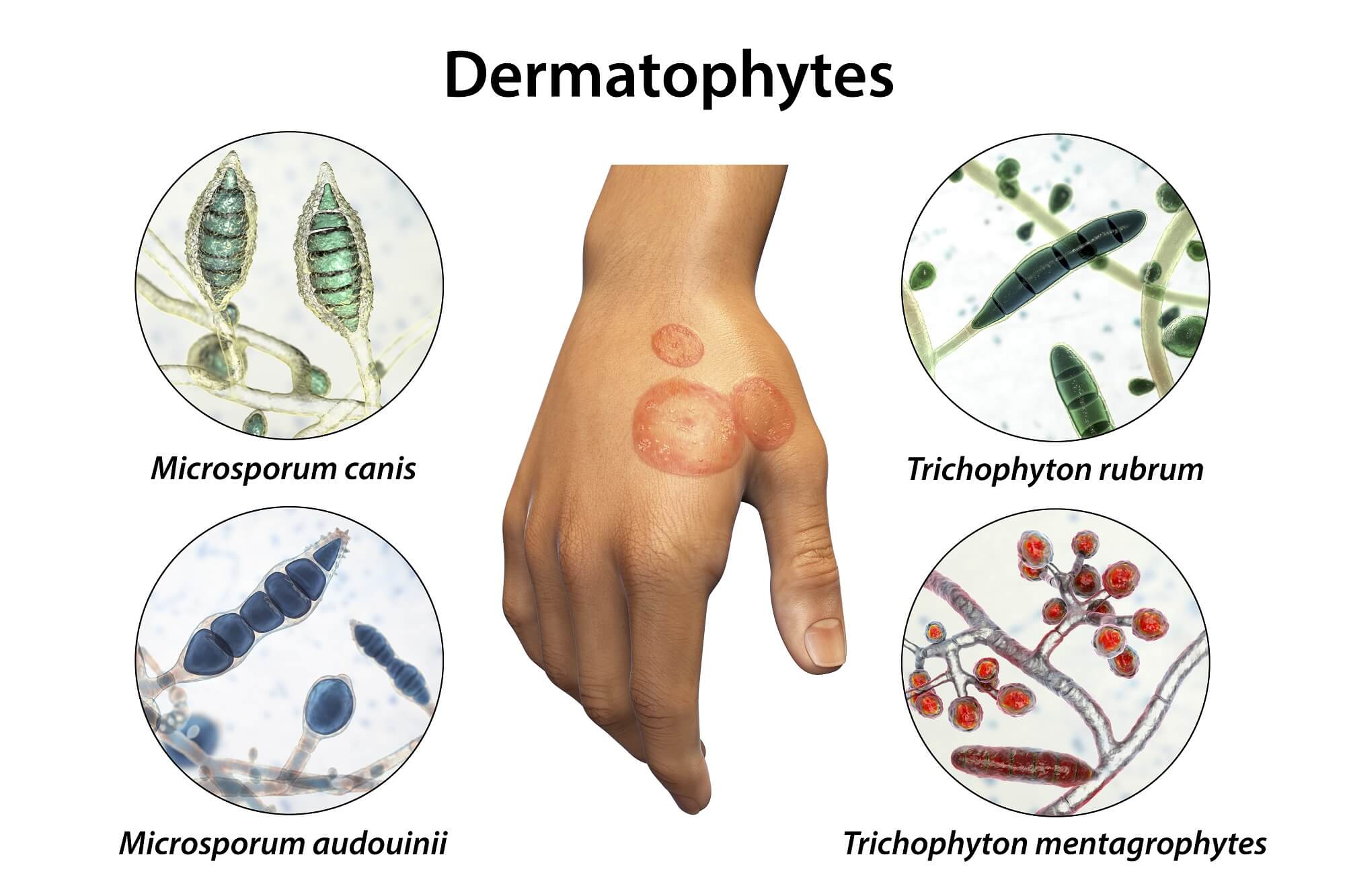
According to the U.S. Centers for Disease Control and Prevention (CDC),(source 1) ringworm has many names. The medical terms for ringworm are "tinea" or "dermatophytosis." Other names for ringworm are given based on the location on the body where the infection occurs.
In this article, we will be referring to ringworm (or tinea) by the term dermatophytosis; as this condition is caused by molds classified as "dermatophytes."
According to a study published in Current Fungal Infection Reports [9.3 (2015): 164-179],(source 2) dermatophytes are one of the most common causes of skin diseases in the world; and the true prevalence is probably underestimated. Dermatophytosis affects about 25% of the world population.(source 3)
A 2015 study in Research in Microbiology(source 4) stated fungal skin diseases caused by dermatophyte molds are among the most common infectious diseases affecting quality of life. The sources of these infections are: other humans, animals, and the soil. These fungal pathogens have the ability to utilize keratin (fibrous structural protein of the hair, nails, and cells in the outer layers of the skin); therefore are found in a variety of places. They cause infection by direct or indirect contact.
This study goes on to say the Dermatophyte family contains over 40 different species in 3 genera: Trichophyton, Microsporum and Epidermophyton. The fungus Trichophyton rubrum (T. rubrum) is the most common dermatophyte in nail and skin infections, it is present in 80 to 90% of disease cases.
Trichophyton mentagrophytes (T. mentagrophytes) is found in 11% of dermatophyte skin and nail infections; and, Epidermophyton floccosum (E. floccosum) in about 7% of these infections.

Comprehensive Herbalist School
Dr. Patrick Jones, founder of the HomeGrown Herbalist School of Botanical Medicine has been a practicing veterinarian for over 25 years. He is also a clinical herbalist and traditional naturopath.
Kevin Harrington, Original Shark from ABC’s Shark Tank, stands behind Dr. Patrick Jones and HomeGrown Herbalist.
Learn More
Comprehensive Herbalist School
Dr. Patrick Jones, founder of the HomeGrown Herbalist School of Botanical Medicine has been a practicing veterinarian for over 25 years. He is also a clinical herbalist and traditional naturopath.
Kevin Harrington, Original Shark from ABC’s Shark Tank, stands behind Dr. Patrick Jones and HomeGrown Herbalist.Learn More
Aloe vera’s Effects on Trichophyton
A 2009 study in the Journal of Medicinal Plants Research(source 5) tested Aloe vera against dermatophytes. The study made two different extracts from Aloe vera; one from water and another from ethanol (drinking alcohol). These extracts were used to test against T. mentagrophytes and T. rubrum.
The study analyzed how toxic various plant extracts, among which was aloe vera, were on the dermatophytes by seeing how the extract would inhibit growth after 5, 10, and 15 days.
After 5 days in contact with the extracts, the following inhibition was seen:
Aloe vera Water Extract (10 mg/L concentration)
- For T. mentagrophytes: 47%
- For T. rubrum: 72%
Aloe vera Ethanol Extract (2 mg/L concentration)
- For T. mentagrophytes: 100%
- For T. rubrum: 100%
Therefore we can see from this study that an ethanolic extract of Aloe vera appears to be drastically more antifungal against T. mentagrophytes and T. rubrum than a water-based extract.
A 2004 study in Pharmaceutical Biology(source 6) investigated how garlic (Allium sativum), black nightshade (Solanum nigrum), and also Aloe vera would affect common dermatophytes and other fungi.
The study made water and 95% ethanol extracts from Aloe vera leaf latex. These two extracts were then tested against several microscopic fungi.
It should be noted that the latex of Aloe vera is different from the gel of the inner leaves. The U.S. National Institute of Environmental Health Sciences(source 7) states that the latex comes from the pulp of the leaves—found just beneath the green cuticle (rind). The latex from Aloe vera is a very powerful laxative.
The study used stock solutions of each extract that had a concentration of 100 mg/mL. These stock solutions were diluted to find the minimum inhibitory concentration (MIC; the lowest concentration that will stop the growth of an organism).
The following MIC levels were found for the water extract of Aloe vera:
- For T. rubrum: 1:500 dilution
- For T. mentagrophytes: 1:500 dilution
- For Aspergillus fumigatus: 1:500 dilution
The following MIC levels were found for the ethanolic extract of Aloe vera:
- For T. rubrum: 1:500 dilution
- For T. mentagrophytes: 1:500 dilution
- For Aspergillus fumigatus: 1:500 dilution
For other tests, it was evident that the ethanolic extracts of the plants were better antifungals than the water based extracts. The study makes the following remarks in its discussion:
Some very interesting outcomes were noted in this study. The ethanol extracts of all the plants were noted to possess more [antifungal] effects as compared to the aqueous extracts.
The high zones of inhibition noted in the ethanol extracts of Solanum nigrum, Aloe barbadensis, and in Allium sativum (using a 1:10 concentration) suggest further explanation of the possibility of using these plants against certain skin infections caused by the above fungal organisms.
Pharmaceutical Biology [42.7 (2004): 491-498]

HomeGrown Herbalist Herb Shoppe
Owner of HomeGrown Herbalist Dr. Patrick Jones is a practicing veterinarian, Clinical Herbalist, and traditional naturopath. He owns and operates Fairview Animal Hospital in Buhl, ID.
Their herb shoppe provides herbs, essential oils, and tools. If you have some time, check it out!
Learn More
HomeGrown Herbalist Herb Shoppe
Owner of HomeGrown Herbalist Dr. Patrick Jones is a practicing veterinarian, Clinical Herbalist, and traditional naturopath. He owns and operates Fairview Animal Hospital in Buhl, ID.
Their herb shoppe provides herbs, essential oils, and tools. If you have some time, check it out!Learn More
A 2021 study in BMC Complementary Medicine and Therapies(source 8) evaluated the antifungal ability of Aloe vera gel against several fungi including Trictophyton species. Additionally, the study combined Aloe vera gel with the following commercially available antifungal creams: clotrimazole (1%), fluconazole (0.5%), terbinafine (1%), and ketoconazole (2%). The combination of the Aloe vera gel and creams were evaluated for a synergistic effect.
Some of the tested fungi included T. rubrum, Trichophyton violaceum (T. violaceum), and T. mentagrophytes.
The following ZOIs were found for Aloe vera gel at a concentration of 10 mg/mL:
- For T. rubrum: about 11.7 mm
- For T. violaceum: about 8.7 mm
- For T. mentagrophytes: about 9.0 mm
The study found there was no synergy or antagonistic effect from combining the antifungal creams with Aloe vera gel on the species of Trichophyton tested.
Claire Goodall’s Amazing Guide
Clair Goodall is a bee-obsessed, natural medicine convert from Minnesota (USA). And, she does keep bees!
Clair has created 350+ page book documenting how to replace the toxic products and medications in your home with healthier, all-natural alternatives.

Aloe vera for Yeast Infections (Candida)
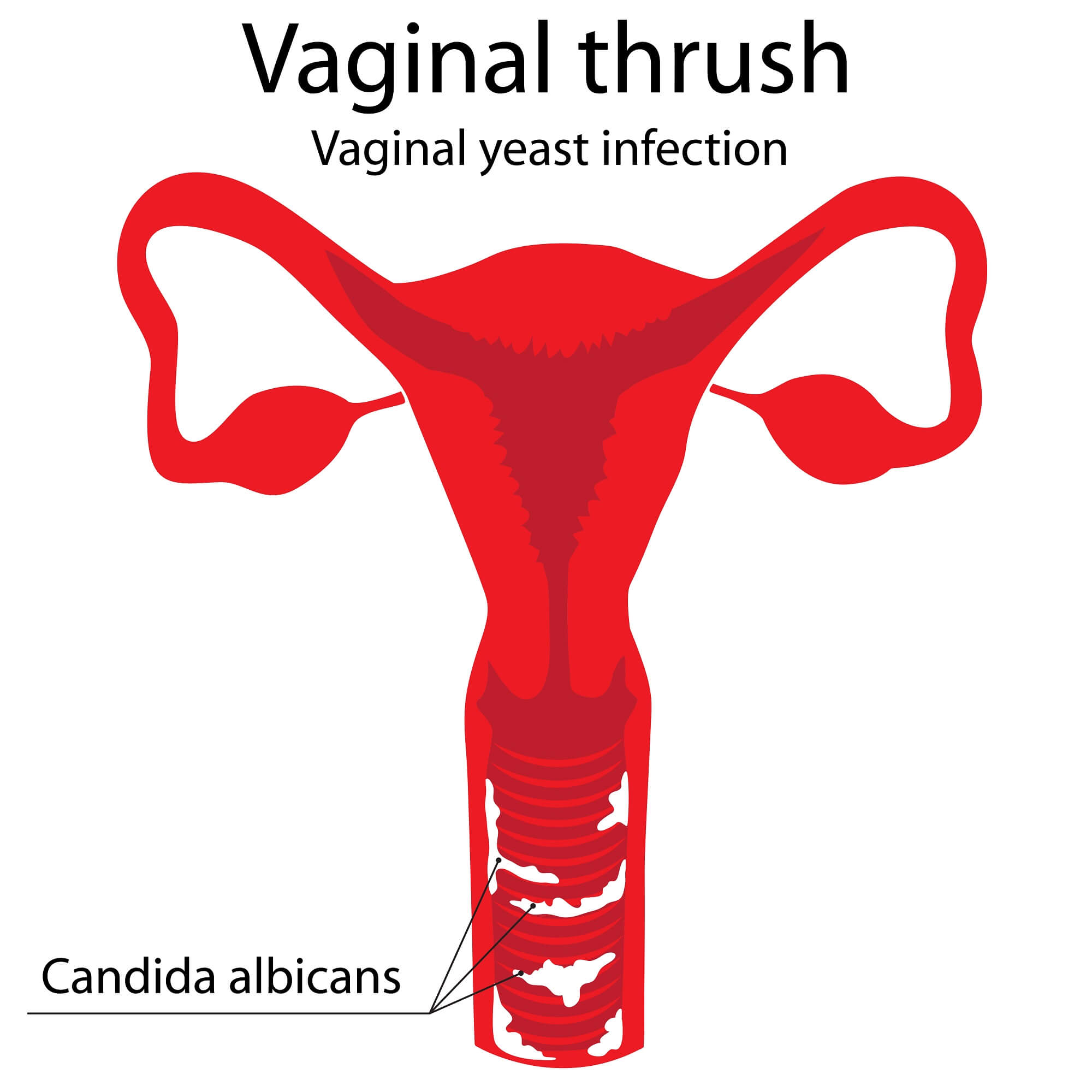
Candida is the genus of yeast that typically causes yeast infections and oral thrush. It can also cause fungal infections of the nails. It is quite a ubiquitous pathogen; and for people at risk (such as having a compromised immune system) it can cause life-threatening infections.
According to the U.S. CDC,(source 9) Candida is a type of yeast, and some of the species in the genera cause infections in people. The most common species to cause infections in people is Candida albicans (C. albicans). Candida normally lives in various places in the body (mouth, gut, vagina) without causing problems; but, when presented with an opportunity, it overgrows causing infection.
The U.S. National Library of Medicine StatPearls article(source 10) also states C. albicans is the most common cause of Candidiasis (Candida infections). Yet, more recently, there has been an increase in other Candida species causing infections.
Possibly the preponderance of studies lists C. albicans as the major cause of Candidiasis, yet these numbers often differ to a degree. One study referenced by this StatPearls article,(source 10) put the distribution of Candida species causing infection (approximations) as:
- C. albicans: 44%
- Candida lusitaniae: 19%
- Candida parapsilosis: 13.7%
- Candida glabrata: 8.42%
How Aloe vera Affects Candida
A 2018 study in the African Journal of Microbiology Research(source 11) found the MIC (minimum inhibitory concentration) and the minimum fungicidal concentration (MFC; i.e., the lowest concentration that kills a microorganism) of Aloe vera against C. albicans.
The study made three different extracts of Aloe vera with three different solvents: ethanol, water, and methanol. The leaves of the Aloe vera plant were chopped, dried, and ground into a powder before the solvents were applied. The solvents were removed before testing the extracts against C. albicans.
The study found the following ZOIs (zones of inhibition) for Aloe vera against C. albicans:
- Ethanol extract: 23mm
- Methanol extract: 12mm
- Water extract: no inhibition zone formed
The study found that both the MIC and MFC for the ethanol extract was in a range between 25 mg/mL to 100 mg/mL.
The study found that both the MIC and MFC for the methanol extract was in a range between 50 mg/mL to 100 mg/mL.
A 2008 study, published in Natural Product Communications,(source 12) examined how Aloe vera would affect various Candida species. This study gives us a more comprehensive idea of how this herb will impact Candida species.
The study used an ethanol and water extract (70:30 ratio) to create their extract. The extract was also further processed and freeze dried for 12 hours. A concentration of 250 mg/mL of Aloe vera extract was used to conduct ZOI tests against Candida species.
The study found the following ZOI’s of the extract:
- For C. albicans: 21.8 mm
- For Candida glabrata: 16.0 mm
- For Candida parapsilosis: no inhibition (interestingly, the antifungal drug amphotericin also produced no inhibition against this species)
- For Candida tropicalis: 16.2 mm
A 2012 study in the the journal Mycoses(source 13) examined how Aloe vera would inhibit the growth of C. ablicans and how it would affect this yeast’s ability to grow germ tubes. The study stated that Candida germ tube formation "represents an essential stage to virulence."
Before discussing this study further, let’s address what Candida germ tubes are. Simply put, some species of Candida can exist in two states: a single yeast cell, or elongated hyphal growths (thin, long tendrils).
C. albicans is one species that grows in these two ways. Hence, C. albicans is said to be dimorphic (occurring in two distinct forms).
One view on this ability of C. albicans to grow in two forms is that it could assist the yeast in penetrating tissue in the early stages of infection. The long hyphal form of the yeast might also be more important for the colonization of organs.(source 14)
Therefore, if an herb can stop the ability of Candida to grow germ tubes and develop into its hyphal form, this may reduce the yeast’s virulence. Hence, it may be very relevant to know an herb’s effects on Candida in this regard.

Comprehensive Herbalist School
Dr. Patrick Jones, founder of the HomeGrown Herbalist School of Botanical Medicine has been a practicing veterinarian for over 25 years. He is also a clinical herbalist and traditional naturopath.
Kevin Harrington, Original Shark from ABC’s Shark Tank, stands behind Dr. Patrick Jones and HomeGrown Herbalist.
Learn More
Comprehensive Herbalist School
Dr. Patrick Jones, founder of the HomeGrown Herbalist School of Botanical Medicine has been a practicing veterinarian for over 25 years. He is also a clinical herbalist and traditional naturopath.
Kevin Harrington, Original Shark from ABC’s Shark Tank, stands behind Dr. Patrick Jones and HomeGrown Herbalist.Learn More
Considering the 2012 Mycoses(source 13) study again, the researchers used a crude glycolic extract of the resinous compound from the outer membrane of fresh Aloe vera leaves.
The study found that C. albicans, in the presence of 10% Aloe vera extract, had an inhibition of approximately 90% of all growth.
C. albicans was also pre-incubated with 10% Aloe vera extract for 30 or 60 minutes. After this initial incubation, C. albicans cells were allowed to grow in goat serum. The pre-incubation was able to reduce germ tube formation. This reduction was seen more when extract pre-incubation was 60 minutes.
When C. albicans was exposed to Aloe vera extract, and germ tube growth was induced, a reduction in cells forming germ tubes was seen. C. albicans in the presence of a 10% concentration of the extract had almost no germ tube formation. Control cultures of C. albicans (without any Aloe vera) had germ tube formation rates of about 70%.
Does Aloe vera Treat Nail Fungus?

Nail fungus, medically termed "onychomycosis," is a condition that can probably be helped by Aloe vera. This is because the fungus T. rubrum causes approximately 90% of all nail fungus infections.(source 15)
Since research has demonstrated Aloe vera is able to inhibit the growth of T. rubrum, it is easy to infer it will help with nail fungus.
According to a 2013 paper in Seminars in Cutaneous Medicine and Surgery(source 15) T. rubrum is estimated to be responsible for about 90% of all nail fungus infections. Most of the rest of these infections are thought to be caused by T. mentagrophytes.
Yet, a number of organisms may also be involved in nail fungus. Yeasts can play a role too, especially Candida.
Candida is most commonly seen in fungal fingernail infections. Candida often causes these infections in tropical regions.
Because Aloe vera can effectively stop Candida, as well as T. ruburm, it is an herbal remedy to consider for using to get rid of nail fungus. It would probably be wise to make or buy an ethanolic extract of Aloe vera to use for this purpose; as it should be a much more powerful antifungal.
But, Aloe vera by itself is probably not the best way to treat nail fungus. Instead, use additional antifungal herbs and essential oils along with Aloe vera.
And, Aloe vera makes a great carrier base for essential oils! This should provide a more antifungal remedy than only Aloe vera.
The Possible Side Effects of Aloe vera
The side effects of Aloe vera is a topic that is beyond the scope of this article. Herbsey does have an entire article on this topic. If you want an evidence based overview of side effects and contraindications, check out the article on this: Aloe vera Side Effects.
Aloe vera is an herb that has been used since antiquity; hence, it has a long history of use by many culture’s traditional medicine. And, as research will demonstrate, topical application is generally well tolerated. The most probable side effects for external use are due to allergic reactions.
Internal use can be done, but there are more precautions to be aware of. And, prolonged ingestion of Aloe vera, especially the inner juice (also known as the “latex”), should be avoided. The latex is such a powerful laxative that you really need to exercise caution with it!
Some quick guidelines for internal use, i.e. cases where Aloe vera should be avoided:
- You are pregnant
- You are taking anticoagulant medications
- You have kidney or cardiac problems
- You have any known allergy to plants in the lily (Liliaceae) family
About the Author
Geoff Kent is a natural medicine enthusiast who has been researching and writing about natural medicine since 2008. Geoff is primarily a web developer, but also researches and authors written and video content about natural health. Geoff has a bachelor’s degree in Management Information Systems from the University of Northern Iowa.
More on Geoff KentImportant Disclosures & Disclaimers
It is important to use the information you find on Herbsey.com in the right way. Also for legal reasons, these disclaimers and disclosures are necessary. For further information about each, feel free to click the link provided to the page on this website that provides more information.
Medical Disclaimer
The information on this website is not a prescription for anyone. This information is for informational or educational purposes only, and is not a substitute for professional medical advice or consultations with healthcare professionals.
Advertisement Disclosure
Some of the links provided on this article and website are affiliate links. If you purchase a product after clicking on these links, Herbsey.com will earn a commission. Herbsey.com promotes various products through advertisement and text links. For more information: Our Advertisements.