Peppermint (Mentha piperita) is a widely used herb, and there are many different forms of the herb (ie, raw herb, leaf extract, tea, and essential oil). Peppermint as a spice has the United States FDA’s recognition of GRAS (generally recognized as safe) status.(source 1) And, the essential oil of this herb also has GRAS status.(source 11)
The renowned, and late, Dr. James Duke (view more about Dr. Duke at the USDA), discusses this peppermint in his book The Green Pharmacy Herbal Handbook.(source 2) Dr. Duke gives peppermint his highest safety rating; stating peppermint is safer to use than coffee. Dr. Duke compares herbs to coffee; and, this is a great idea because who isn’t familiar with coffee?
Although this herb is therefore probably very safe, as worldwide use can attest to, problems can occur with it; especially if you use it at therapeutic doses or use the essential oil. In this article, we will discuss the commonly reported side effects and provide dosage suggestions for this popular herb.
Perhaps most important to note is that if you are pregnant you should not use peppermint as it is an emmenagogue; i.e., it stimulates menstruation. And, small children and infants should not use peppermint oil as serious side effects may be possible.
You may want to consult a medical professional before using peppermint if you are taking certain prescription drugs. This is because peppermint inhibits certain kinds of enzymes that are in the Cytochrome P450 family; and, these enzymes are responsible for breaking down foreign substances (such as prescription drugs) in the body. The inhibition of certain Cytochrome P450 enzymes can lead to more of a medication in your system than should normally be there.
If you don’t have much time, listed below is a good list of potential side effects and hazards to be aware of before you start using peppermint.
Summary of General Side Effects of Peppermint
- Gastrointestinal Side Effects
- Peppermint is a choleretic (something that induces bile secretion by the liver) and should be avoided by people with bile duct inflammation or obstruction.(source 4)(source 6)
- Fast releasing peppermint oil can cause heartburn.(source 4)
- Skin Contact Side Effects
- Can cause dermal irritation and sensitization.(source 3)(source 4)(source 5)
- Menthol can cause burning sensations at concentrations of 5% or more.(source 3)
- Oral Side Effects
- Aggravation or causation of oral lichenoid reactions, stomatitis, burning mouth syndrome (BMS), recurrent oral ulcers, and perioral dermatitis.(source 3)
- Worsening of asthma when using peppermint orally.(source 5)
- Side Effects in Children
- Direct use of peppermint oil to the chest or nasal area of infants may cause bronchial spasms, laryngeal spasms, or a sudden cessation of breathing (apnea).(source 16)(source 11)(source 6)
- Side Effects During Pregnancy
- Peppermint should be avoided in early pregnancy due to its ability to stimulate menstruation.(source 6)
Dr. John Herzog (MD)
Dr. John Herzog, a "survival surgeon" from Maine explains what home remedies work best in a crisis situation.
This may be important in the event you require first-aid or are in an emergency situation without easy access to a hospital. Dr. John Herzog has assembled a large collection of home remedies for such scenarios.

General Side Effects & Contraindications

According to a 2010 study in Dermatitis(source 3) pulegone (a chemical in peppermint) is known to be toxic to the liver (scientific term: hepatotoxin). We now know that this chemical is also neurotoxic as well.(source 16) Pulegone is present in young peppermint leaves and is later metabolized to menthol.
Peppermint oil, depending on how it is made, can have a concentration of pulegone in it ranging from 1% to 4%. Because of this chemical’s toxicity, pulegone is limited to 1% or less. This is especially important as menthol has been demonstrated to enhance the penetration and absorption of other chemicals.
The study also reports that because peppermint oil can cause skin irritation and sensitization, patch testing (taking a small amount of a substance and applying it to an insensitive area of the skin for a period of time to observe if any reaction takes place) with a 2% concentration of peppermint oil in a carrier base should be done before using this oil.
The study also goes on to say that menthol can cause burning sensations at concentrations of 5% or more.
People with oral lichenoid reactions, stomatitis, burning mouth syndrome, recurrent oral ulcers, and perioral dermatitis have had these conditions aggravated by both peppermint oil and menthol. Several patients with these conditions who avoided menthol and peppermint oil found their symptoms to cease. This cessation could happen within as little as 3 days.
Additionally, some of these patients had reported symptoms lasting up to 8 years, which subsequently ceased when they maintained an avoidance routine.
A 2007 paper in Medicine Today(source 4) stated peppermint oil can cause contact dermatitis (a rash due to an allergic reaction to a substance or direct contact with it), especially for people with aspirin-induced asthma.
The study also relates an established fact that peppermint oil is a choleretic (something that induces bile secretion by the liver) and should be avoided by people with bile duct inflammation or obstruction.
The study also states fast releasing peppermint oil can cause heartburn (gastroesophageal reflux). Yet, this is unlikely if a person is using enteric-coated peppermint oil.
Concerning heartburn, the 2007 study in American Family Physician(source 6) study states:
Peppermint oil is relatively contraindicated in patients with hiatal hernia or significant gastroesophageal reflux disease, because its effect on the lower esophageal sphincter can lead to exacerbation of symptoms.
American Family Physician [75.7 (2007): 1027-1030]
A 2001 study in The Journal of the Royal Society for the Promotion of Health(source 5) also discussed the side effects of peppermint. The study said it may cause heartburn, and rare side effects include idiopathic atrial fibrillation (irregular, often rapid heartbeat that can cause blood clots in the heart; idiopathic means there is no clear cause for this condition).
The study cites two cases of idiopathic atrial fibrillation that occurred in people who were addicted to sucking peppermints; and this condition went away when they stopped using the peppermints.
Claire Goodall’s Amazing Guide
Clair Goodall is a bee-obsessed, natural medicine convert from Minnesota (USA). And, she does keep bees!
Clair has created 350+ page book documenting how to replace the toxic products and medications in your home with healthier, all-natural alternatives.

Side Effects During Pregnancy

According to a 2007 study in American Family Physician,(source 6) peppermint oil has been used to induce menstruation; therefore, it should not be used during pregnancy. A 2015 study in the Oman Medical Journal(source 7) also states that peppermint should be avoided in early pregnancy due to its ability to stimulate menstruation.
Concerning preterm birth, a 2010 study in the European Journal of Obstetrics and Gynecology and Reproductive Biology(source 8) investigated the use of several herbs and this problem. The study defined a preterm birth as one occurring before the 37th week of pregnancy. Women investigated were in the last two trimesters of pregnancy; i.e., greater than 15 weeks of gestational age. 3,191 women participated in this study.
Among women with preterm births, peppermint was used by 2.09% of them. The study found no relationship between using peppermint and preterm birth. The only herb among the few that were studied that showed an increased risk of preterm birth was flax. Taking flax had an odds ratio of 3.91 (meaning that those who took flax were about 3.91 times more likely to have preterm births).
Another study, published in 2022 in Pharmaceutics,(source 9) reviewed literature regarding certain herbs and their use during pregnancy. Peppermint was one of the investigated herbs.
The study discussed the risk of teratogenic (developmental malformations) effects from peppermint use during pregnancy. The study cited an experimental study that gave peppermint at doses of 600 and 1,200 mg / kg of body weight per day to pregnant mice during the embryonic period. The cited research found no serious congenital developmental problems or delayed bone formation in the fetuses. Thus, this cited research showed that peppermint might not have any developmental malformations for mice.
This literature review in Pharmaceutics(source 9) also stated that peppermint at normal doses has been seen as safe for pregnant women. The study lists 5 studies that encompassed a total of 3,031 participants using peppermint during pregnancy. 3 of these studies stated that there were no side effects reported; the other two did not even mention side effects.
It should be noted that the American Family Physician(source 6) study also stated that peppermint in typical products is likely safe for pregnant women, the paper states:
However, the amount of peppermint in over-the-counter medications, topical preparations, and herbal teas is likely safe in pregnant and lactating women and in young children.
American Family Physician [75.7 (2007): 1027-1030]
Side Effects with Infants

A 2020 study in the International Journal of General Medicine(source 10) stated peppermint oil is known for its toxic effect on children. This study cites a clinical case report demonstrating medication which had peppermint oil as a flavoring additive caused effects such as atrial fibrillation (irregular, frequently rapid heart rate that can cause poor blood flow) and digestive problems in children. This study also states this substance can cause muscle pain and burning sensations in children.
A 2008 study in the Journal of Herbal Pharmacotherapy(source 11) states that peppermint oil can be unsafe for infants and small children. According to this paper, oral peppermint oil has caused infants and small children to experience the following adverse reactions:
- Acute respiratory distress with cyanosis (when the lips, skin, and nail beds turn blue due to a lack of oxygen in the blood)
- Respiratory arrest
- Tongue spasms
- Temporary stopping of breathing (scientific term: apnea)
- Laryngeal and bronchial spasm
Also important to note, according to this same study, peppermint is likely to be safe for children when ingesting amounts commonly found in foods. And, the study reports that peppermint oil is Generally Recognized as Safe (GRAS) by the United States Food and Drug Administration.
The 2007 American Family Physician study(source 6) cites the Expanded Commission E Monographs and reports that peppermint oil should not be used near the face or used internally with infants or young children. This is due to the potential to cause respiratory arrest, tongue spasms, and bronchial spasms.
Drug Interactions due to Cytochrome P450
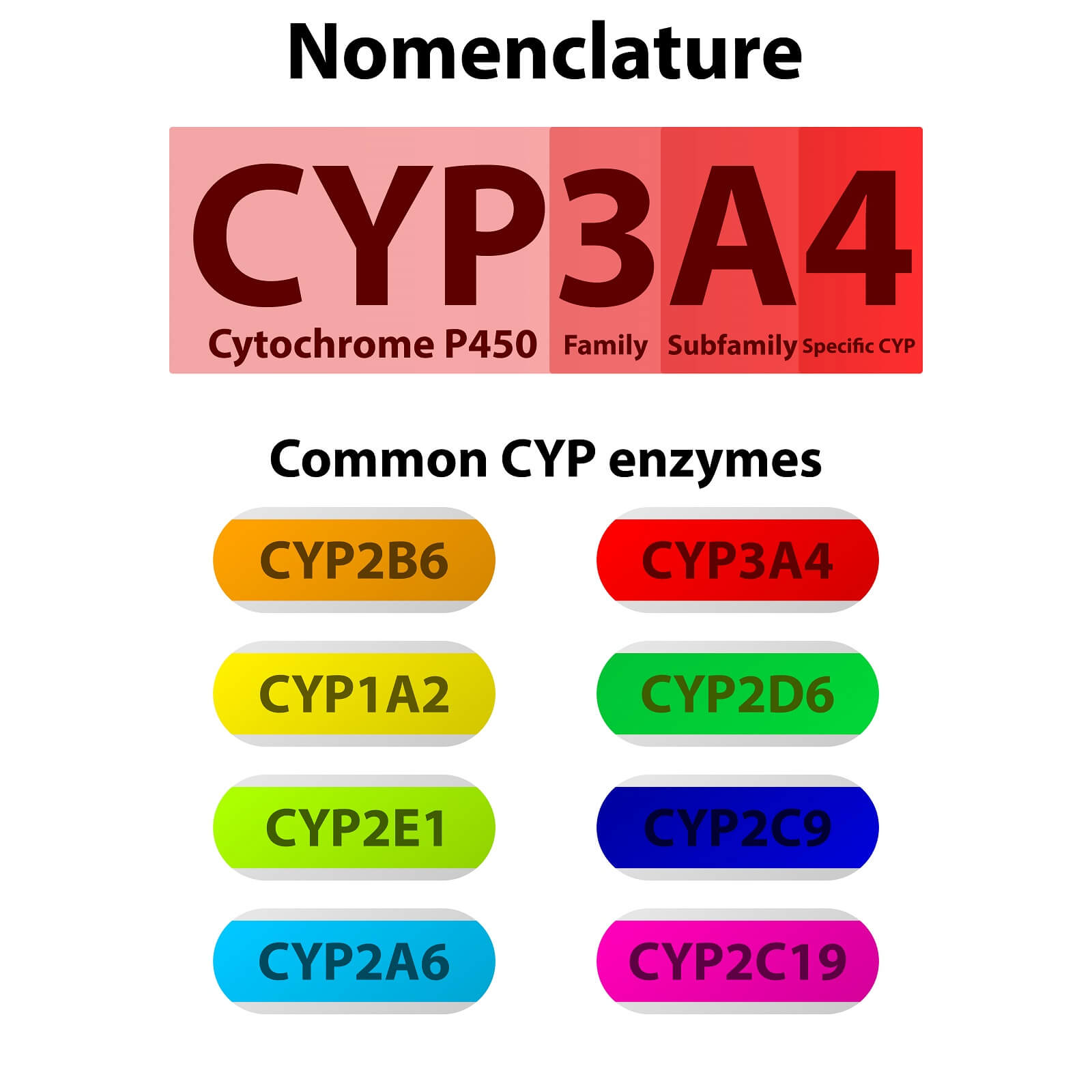
One important question to consider before you take an herb medicinally, is does it interact with cytochrome P450 isoenzymes (CYP). Let’s explain quickly what CYP is and why it is important to consider for assessing the possibility of drug interactions.
According to a 2014 study in the EXCLI Journal 13(source 18) there have been many mechanisms for herbal drug interactions suggested. Yet, a common way herbs interact with synthetic drugs is by changing the absorption, metabolism, or elimination of the drug. The phytochemicals in these herbs can influence metabolizing enzymes like CYP.
CYP is a heme protein that has a crucial role in the metabolism of drugs and other chemicals foreign to the body (i.e., xenobiotics).(source 12) Heme proteins are among the most versatile of metalloproteins.(source 13) Metalloproteins (metal-binding proteins) are very common in biological systems. In the majority of metalloproteins, the metal ion provides a specific biological function.(source 14)
According to a 2007 study in American Family Physician,(source 15) CYP is essential for metabolizing many drugs. The following quote from this study discusses this:
Cytochrome P450 enzymes are essential for the metabolism of many medications. Although this class has more than 50 enzymes, six of them metabolize 90 percent of drugs, with the two most significant enzymes being CYP3A4 and CYP2D6...
Cytochrome P450 enzymes can be inhibited or induced by drugs, resulting in clinically significant drug-drug interactions that can cause unanticipated adverse reactions or therapeutic failures. Interactions with warfarin, antidepressants, antiepileptic drugs, and statins often involve the cytochrome P450 enzymes.
American Family Physician [76.3 (2007): 391-396]
A 2021 study in Toxin Reviews(source 16) stated that peppermint essential oil could stop the CYP enzyme CYP3A in vitro (in a test environment, not in a living subject) in human and rat livers. This led to the essential oil inhibiting the metabolism of cyclosporine (an immunosuppressive drug; common brands: Gengraf, Neoral, and Sandimmune) metabolism in vitro.
Because CYP3A is an important CYP enzyme, it may be that peppermint will stop the metabolism of other drugs as well. Consequently, make sure to talk to a medical professional before you start taking peppermint therapeutically.
Peppermint Dosage Guidelines
A 1999 study in Hospital practice(source 17) discussed peppermint dosage guidelines. The study recommended:
- 6 to 12 drops of tincture once a day.
- 1 to 2 enteric-coated capsules (0.2 mL) 3 times a day (between meals for irritable bowel syndrome).
Dr. James Duke, in his book The Green Pharmacy Herbal Handbook,(source 2) gives dosage guidelines for peppermint which are as follows:
- 1 dropper of concentrated extract or tincture (not the essential oil) per day.
- Tea made from 1 tablespoon of fresh leaves in 1 cup of hot water; up to 4 times per day.
- Tea made from 1 to 2 teaspoons of dried leaves in 1 cup of hot water; up to 3 times per day.
- 1 to 2 enteric-coated capsules (containing 0.2 mL of the essential oil) 3 times a day.
Dr. Duke also states that if you are using peppermint oil capsules, make sure you get the enteric-coated type. This allows the essential oil to survive the harsh conditions in the stomach and reach the intestines. Once in the intestines, the peppermint oil can then relax the smooth muscles of this organ.
About the Author
Geoff Kent is a natural medicine enthusiast who has been researching and writing about natural medicine since 2008. Geoff is primarily a web developer, but also researches and authors written and video content about natural health. Geoff has a bachelor’s degree in Management Information Systems from the University of Northern Iowa.
More on Geoff KentImportant Disclosures & Disclaimers
It is important to use the information you find on Herbsey.com in the right way. Also for legal reasons, these disclaimers and disclosures are necessary. For further information about each, feel free to click the link provided to the page on this website that provides more information.
Medical Disclaimer
The information on this website is not a prescription for anyone. This information is for informational or educational purposes only, and is not a substitute for professional medical advice or consultations with healthcare professionals.
Advertisement Disclosure
Some of the links provided on this article and website are affiliate links. If you purchase a product after clicking on these links, Herbsey.com will earn a commission. Herbsey.com promotes various products through advertisement and text links. For more information: Our Advertisements.